Characterizing adaptive immune response in emphysema patients to better inform personalized treatments
With a $3.3M dollar grant from the National Institutes of Health, Dr. Francesca Polverino will investigate unique B cell responses in patients with emphysema, a subtype of chronic obstructive pulmonary disease (COPD).
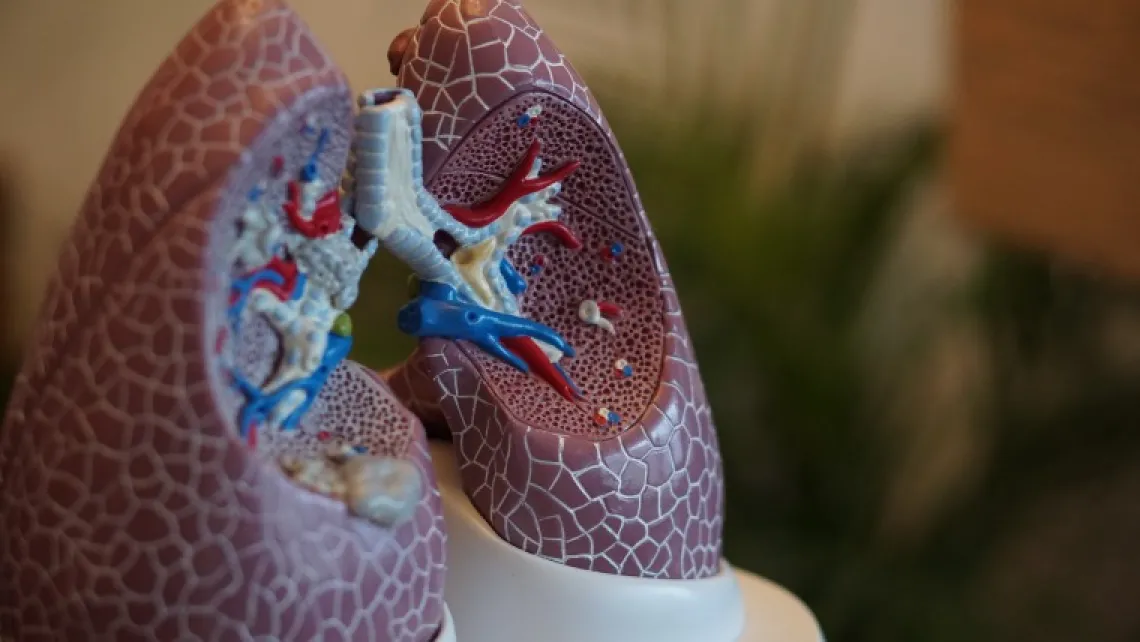
Francesca Polverino, a BIO5 Institute member and University of Arizona associate professor of medicine, has been awarded $3,364,046 from the National Heart, Lung, and Blood Institute to study an emerging hallmark of emphysema, a lung condition that causes shortness of breath and often leads to chronic obstructive pulmonary disease (COPD). The five-year grant will allow Polverino and her colleagues to characterize the unique immune response associated with emphysema, ultimately informing earlier and more personalized treatment approaches.

COPD is the third leading cause of death in the U.S. and world and causes lungs to irreversibly lose their elasticity, making it difficult to completely exhale with each breath.
The progressive, inflammatory disease is multifactorial in nature with not only environmental contributors, but genetic and developmental factors, as well. Tobacco smoke is the most prominent risk factor in developed countries like the U.S., while inhalation of smoke generated by burning fuels indoors is key for underdeveloped countries around the globe.
Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD. Current treatments including lifestyle changes, prescription medication, breathing therapies and surgery are used for both. Because the two diseases are inherently different, however, Polverino insists that distinctive approaches must be taken. So far, a therapy modifying the course of COPD has not been found.
“People with emphysema cannot be encompassed under the same umbrella as other COPD patients because they present a completely different disease,” said Polverino, also an associate professor of physiological sciences and associate research scientist with the UArizona Health Sciences Asthma & Airway Disease Research Center.
Unlike those with chronic bronchitis, emphysema patients exhibit autoimmune responses leading not only to loss of lung tissue, but also to loss of bone and muscle throughout their bodies. These patients are “falling apart systemically,” likely because of improper B cell responses.
B lymphocytes, a key part of the adaptive immune system, are white blood cells responsible for producing antibodies in response to foreign materials and harmful microbes. While the actions of B cells are essential to our protection against a variety of diseases, they sometimes incorrectly target our own tissues, leading to an autoimmune response.
Work by Polverino and others has shown that not all COPD patients – only those with emphysema – have prominent lung B cell responses, regardless of the degree of airflow limitation they experience.
With this new grant, the physician-scientist will further explore the B cell immune responses in COPD patients, especially those with emphysema and heightened autoimmunity.
“This research is the first brick of a wall because we really don’t know anything about the B cell response in these people,” Polverino said. “This work is very overdue.”
Once she correlates the extent of B cell activity with emphysema severity, Polverino plans to assess antibody production throughout the body since emphysema causes systemic (whole-body) problems. If her hypothesis is correct, Polverino expects that circulating off-targeted B cells, similar to that in the lung, will also correlate with emphysema severity.
Though an expert in chronic lung diseases herself, Polverino will also collaborate with other scientists, both at UArizona and other institutions across the U.S., to tackle this project from every possible angle.
BIO5 member Deepta Bhattacharya, also an associate professor of immunobiology, surgery and genetics, will conduct functional B cell assays, while Paul Langlais, an associate professor of medicine and director of the UArizona Proteomics Lab, will assist with the use of a mass spectrometer, a tool used to determine the precise components of a substance. Another BIO5 member and assistant professor of cellular and molecular medicine, Darren Cusanovich, will perform single-cell sequencing to determine the genetic differences between B cells in COPD patients. Jin Zhou, associate professor of epidemiology, will assist Dr. Polverino with the biostatistical analyses required for her project.
Through their work, Polverino and her cross-disciplinary team aim to identify biomarkers of emphysema B cell responses that are distinct from other types of COPD. With these specific indicators, scientists and physicians will be able to take a precision medicine approach to treating this chronic disease.
Grant Information
R01 HL149744
Granting Institutions: NIH/NHLBI
Amount: $ 3,569,551
Time Period: 09/2020-09/2025
Title: B cell adaptive immune profile in emphysema-predominant COPD
Principal Investigator: F. Polverino
Researcher Contact
Francesca Polverino, M.D., Ph.D.
Associate Professor, Medicine
Associate Professor, Physiological Sciences
Associate Research Scientist, Asthma & Airway Disease Research Center, UA Health Sciences
Associate Professor, BIO5 Institute
francy@email.arizona.edu
520-626-8485
