Collaborative teamwork untangles complex web of chronic pelvic pain and endometriosis
A pilot study co-led by 2023 BIO5 Postdoctoral Fellow Nicole Jimenez at the University of Arizona College of Medicine – Phoenix brings together a diverse team to lay the groundwork for linking the microbiome to poorly understood gynecologic conditions.
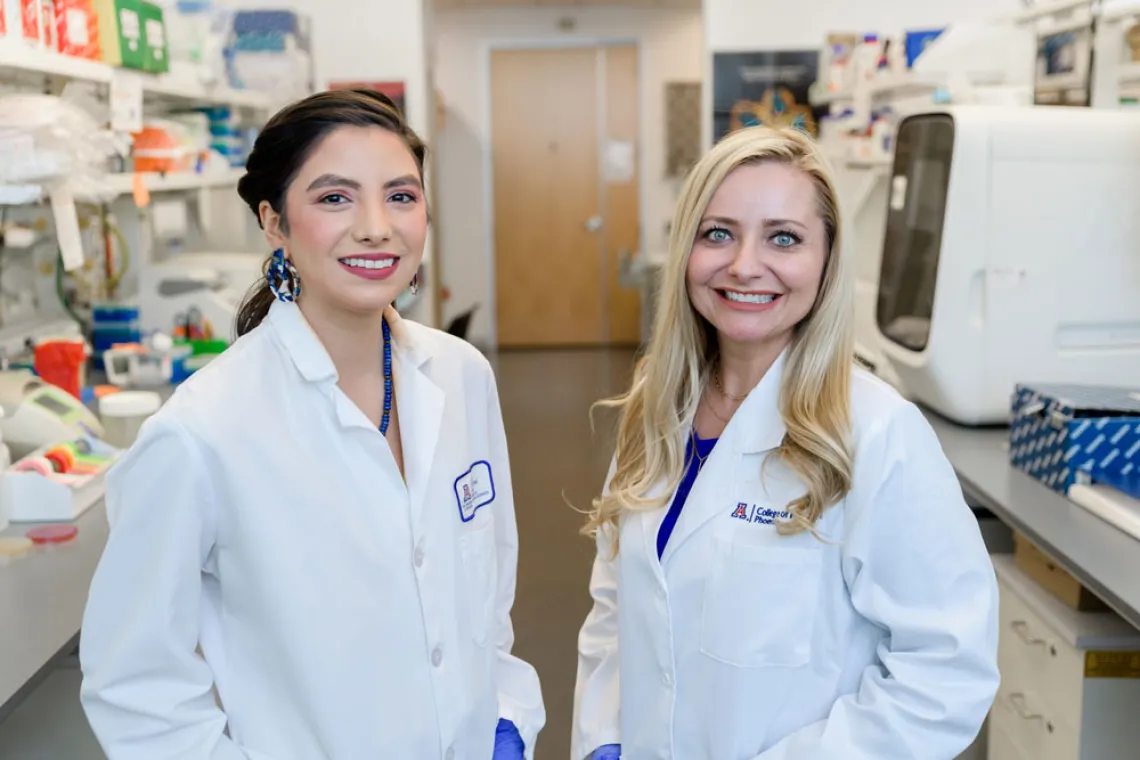
Nicole Jimenez (left), postdoctoral researcher in the lab of BIO5 member Melissa Herbst-Kralovetz (right), is studying the microbiome in hopes to of better understanding chronic pelvic pain and endometriosis at the University of Arizona College of Medicine – Phoenix.
Fostering a collaborative culture to solve critical health problems facing the Arizona community is a core part of the BIO5 Institute mission at the University of Arizona. Women’s health research by BIO5 members is an excellent example of how innovative and interdisciplinary partnerships tackle these complex health challenges.
“Collaboration is a huge focus of our lab,” said Nicole Jimenez, first co-author and postdoctoral researcher in the lab of BIO5 member Melissa Herbst-Kralovetz at the U of A College of Medicine – Phoenix. “Even though we brought together a large team with very different perspectives for this study, everyone has the same focus and commitment to women’s health.”
A paper in BMC Medicine by Jimenez and first co-author Taylor Norton at Banner – University Medical Center Phoenix united translational, clinical, and surgical science to provide critical information on two poorly understood conditions in women’s reproductive health: chronic pelvic pain (CPP) and endometriosis.
The pilot study investigated the vaginal and rectal microbiome of patients suffering from these conditions, revealing significant differences in microbiota that can be used to develop improved diagnostics and personalized treatments. The team of researchers included faculty, postdoctoral researchers, medical residents, and undergraduate and graduate students across the U of A College of Medicine – Phoenix, Mel and Enid Zuckerman College of Public Health, College of Nursing, and Banner – University Medical Center Phoenix.
“Women are complex, and chronic pelvic pain and endometriosis are two conditions that highlight that complex interplay between the microbiome, immune system, and hormones,” said Herbst-Kralovetz, professor of basic medical sciences and director of the Translational Women’s Health Research Program and Microbiome Initiative at the U of A College of Medicine – Phoenix. “We must take a multi-pronged approach to better understanding these conditions.”
Complicated answers from integrated microbiome and immune data
Jimenez, Norton and their transdisciplinary team are driven by the fact that not only do CPP and endometriosis significantly impact a woman’s quality of life, but they are also economic burdens. Those who suffer from these conditions struggle with the high costs of medical treatments, frequent doctor visits, surgeries, and lost productivity from missed work.
Taylor Norton is a first co-author and gynecologic surgeon at Banner – University Medical Center Phoenix.
Chronic pelvic pain is ongoing discomfort in the lower abdomen or pelvis lasting longer than six months, estimated to affect up to 26% of women worldwide. One cause of CPP is endometriosis, affecting 10% of women globally, a painful condition where uterine tissue grows outside the uterus causing inflammation and discomfort. However, there is little research on the link between these conditions.
Researchers examined microbiomes in key regions of the human body that could potentially reveal any connection. The pilot study divided 75 patients into three groups, CPP and endometriosis, CPP only, and no CPP, combining individual microbiome data with patterns of immune system activity for each patient.
This created unique biological "fingerprints” for researchers—now they can understand how specific microbes are associated with certain conditions, as well as how a patient’s body responds.
Findings revealed differences in vaginal microbiota and immune signatures between the groups. But just as important was data that revealed connections with co-occurring conditions, including fibroids, abnormal uterine bleeding, and irritable bowel syndrome (IBS).
“Integrating that microbiome and immune data helped us see how other gynecological conditions were associated with bacterial vaginosis bacteria in the vaginal microbiome and a large number of immune markers,” said Jimenez, a 2023 BIO5 Postdoctoral Fellow.
Another example is a robust signature of microbes associated with IBS in the rectal microbiome. As many patients with endometriosis are often co-diagnosed with IBS, this finding reinforces how it could also be a cause of CPP.
The results gave the team important clues into how to proceed in untangling the complex web between CPP and endometriosis. Luckily, they had built a team with the necessary expertise.
Building a women’s health research dream team
The catalyst for this study started over five years, when Herbst-Kralovetz began working with obstetrician gynecologist (OB/GYN) residents at Banner – University Medical Center Phoenix.
The OB/GYNs wanted better solutions for the current painful and invasive diagnostic for endometriosis. This need led Herbst-Kralovetz and her lab to wonder if microbiological data could provide important clues to this understudied gynecological condition. This was the start of the collaboration with co-first author Norton, then an OB/GYN resident specializing in minimally invasive surgery.
“As a surgeon, I readily acknowledge that surgical treatment of endometriosis is not curative and I long to have additional therapeutic options to offer my patients who deal with this chronic condition,” said Norton, now a gynecologic surgeon. “This study offers additional evidence that there are microbiome and inflammatory marker changes in pelvic pain conditions and endometriosis which, I believe, will lead to breakthroughs in endometriosis diagnosis and treatment.”
Norton’s perspective provided key clinical viewpoints on the data. When Jimenez joined the lab in 2021, she brought with her expertise in microbiome analyses, including her work on the vaginal microbiome in her graduate studies.

Leslie Farland is an associate professor in the University of Arizona Mel and Enid Zuckerman College of Public Health and BIO5 member.
Reviewing microbiome and immune data together, Jimenez and Norton began to see the links between CPP and endometriosis. But as often happens with science, results often lead to more questions than answers.
The data revealed a growing web of interplay with co-occurring conditions, so they recruited another team member to help with the data analyses and interpretations. A reproductive epidemiologist focused on endometriosis, Leslie Farland is an associate professor in the Zuckerman College of Public Health and BIO5 member.
“Before collaborating with the Herbst-Kralovetz lab, I had no experience in the microbiome, but I did have a great deal of experience studying endometriosis,” said Farland. “Through these cross-campus collaborations I believe we’ve been able to conduct more rigorous research to advance women’s health.”
Besides the foundational microbiome data, Farland emphasizes how this work sought to include how even benign gynecologic conditions can influence women’s health.
“The vast majority of prior endometriosis research would dichotomize participants into those who have endometriosis and those who don’t have endometriosis,” said Farland. “However, the reality is that those who don’t have endometriosis may have other gynecologic conditions like fibroids which may influence their health and microbiome. It’s rare for someone to not have any other condition. By only looking at one condition at a time you may be missing important information.”
Bigger grants for expanded analyses
The detailed results showed the team how crucial it was to avoid oversimplifying gynecological conditions.
“As a researcher, we like to put people into distinct buckets,” said Herbst-Kralovetz. “That kind of approach is simply not feasible when it comes to women and their uteruses.”
As a pilot study, this smaller scale research project provides foundational data and knowledge for Jimenez and her collaborators to build on in future research.
They are actively submitting grants using the data from this study with larger and more diverse cohorts. These studies will include more multi-omics approaches (e.g. immunoproteomics, metabolomics, and microbiome profiling), further investigating benign gynecological conditions and considering racial and sociocultural factors.
“We want to not only expand our analyses for better diagnostics and better treatment of symptoms, but also understand these conditions from a community setting and any barriers to seeking care,” said Jimenez, referencing the latter being pursued by her collaborator in the U of A College of Nursing.
The web is complex, but Jimenez, Norton, Herbst-Kralovetz, and their team have the collaborative teamwork to untangle it.
