Combating chronic pain
Several BIO5 researchers address chronic pain, working to tackle the opioid epidemic through basic science and clinical approaches.
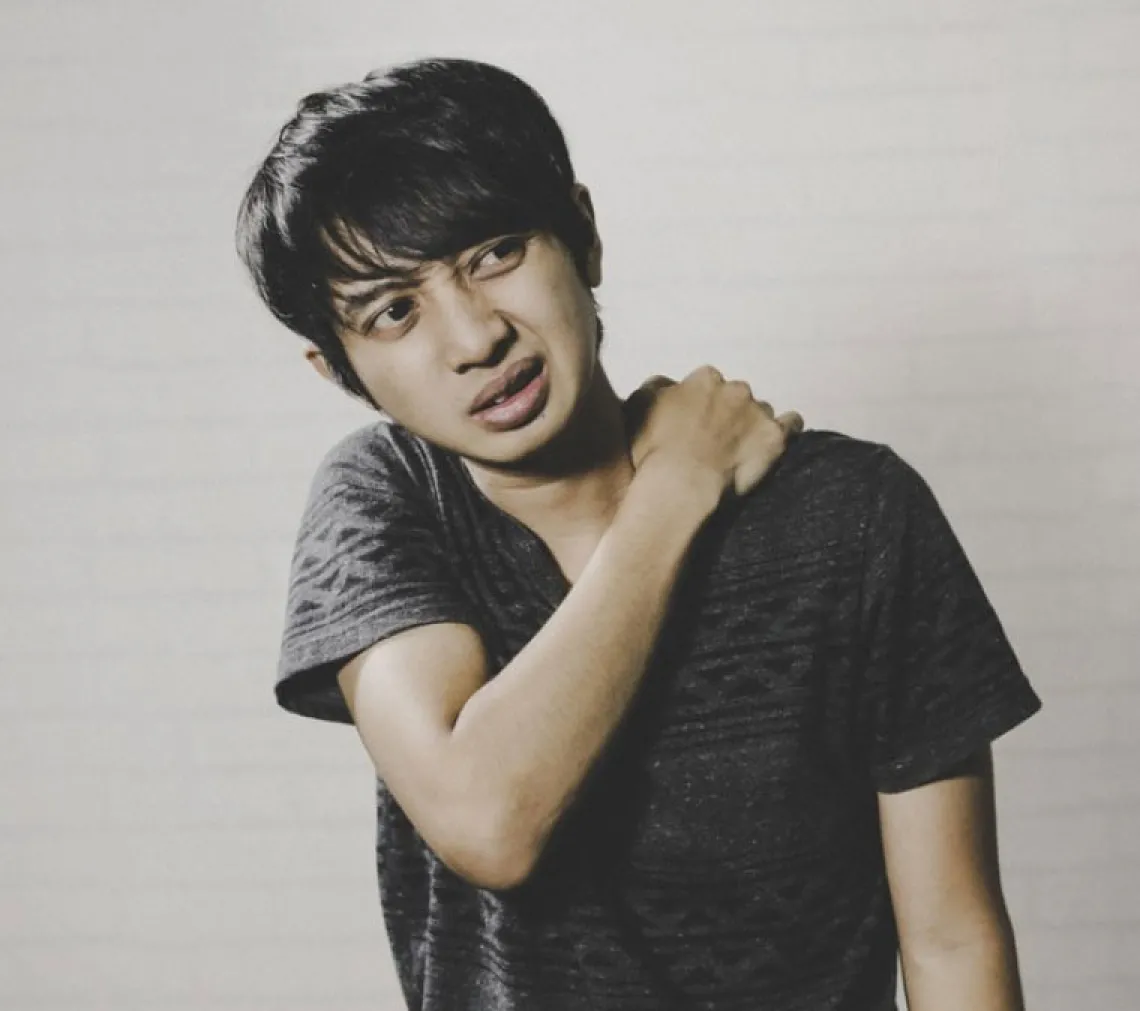
Pain is a normal response to potential injury – but chronic pain is different. Unlike the short-lived discomfort associated with a stubbed toe or papercut, chronic pain lasts weeks, months or even years after the initial injury. Some even experience long-lasting pain in the absence of damage.
More than 1.5 billion people live with chronic pain worldwide, and it’s the most common cause of long-term disability in the United States. Chronic pain severely compromises an individual’s quality of life, limiting mobility and reducing strength, flexibility and endurance.
Prescription medication, acupuncture, brain stimulation and surgery can help to treat this condition, but it’s typically poorly managed. Some addictive treatment modalities like opioids can be misused and abused, leading to severe health and societal consequences.
In 2017, the U.S. Department of Health and Human Services declared a public health emergency to address the opioid epidemic that is responsible for nearly 50,000 deaths annually. Several researchers at the BIO5 Institute are identifying and developing alternative therapies to end the opioid epidemic and provide relief to the billions living with chronic pain.
Vijay Gokhale, a BIO5 associate research professor, develops small molecule therapeutics for neuropathic, or nerve, pain. He, along with May and Rajesh Khanna, invented a new class of non-opioid, non-addictive compounds to treat pain. The team worked with Tech Launch Arizona to patent the technology and develop their startup company, Regulonix, in 2018.
“Addiction to opioids is a major problem in United States. With this technology, we are developing small molecules for chronic pain that will provide safer and nonaddictive treatment options," Gokhale said.
Rajesh Khanna, a professor of anesthesiology, neuroscience and pharmacology, also investigates non-opioid pain targets by studying novel protein interactions and cellular ion channel regulation.
Todd Vanderah, department head of pharmacology and co-director of the MD/PhD dual degree program, recognized a need to unite faculty in the health sciences and BIO5 to significantly tackle opioid use disorder and reduce opioid-induced morbidity and mortality by promoting innovative, non-narcotic ways to help those who suffer from chronic pain.
This led to the development of the UArizona Health Sciences Comprehensive Pain and Addiction Center in 2020. The Center aims to address the opioid epidemic through several angles including addiction, chronic pain, education, legislation and research.
“Since starting the Center in 2020, faculty members have achieved over $13 million in new federal grants that include novel targets to inhibit chronic pain, a clinical trial for patients with cancer pain, an addiction-medicine fellowship, training of physicians in medication-assisted treatment, and the University's first program to develop paraprofessionals in serving families with substance use disorder in Pima and Santa Cruz counties,” said Vanderah, also a professor of anesthesiology, neurology, neuroscience, pharmacology and physiological sciences.
In his laboratory, Vanderah investigates the cellular differences between acute and chronic pain, as well as the mechanisms of cancer-induced bone pain. In addition to understanding the molecular details of pain, Vanderah seeks to identify novel targets for drug discovery and test potential therapeutic compounds through his research.
Tally Largent-Milnes, a research assistant professor of pharmacology, and Victor Hruby, a Regents professor emeritus, are also pursuing non-opioid interventions. Largent-Milnes studies mechanisms and treatments for neuropathic, craniofacial (skull and face), and migraine pain. She places special emphasis on methods to pass drugs across the highly regulated blood brain barrier, as this has proven to be an obstacle to treating these types of pain.
Hruby is well-known for developing novel compounds for the treatment of prolonged pain without the toxicities and tolerance of existing options.
Like Largent-Milnes, Thomas Davis, a professor of neuroscience, pharmacology, pharmacology and toxicology, and physiological sciences, is also addressing the permeability of the blood brain barrier. He targets specific cellular signaling pathways and transporters to enhance delivery of drugs to the central nervous system.
Robin Polt, professor of chemistry and biochemistry, neuroscience, and pharmacology and toxicology, studies the biology of cellular membranes. His findings help further the design of new therapeutics that penetrate the blood brain barrier to provide chronic pain relief.
Together, these BIO5 researchers are paving the way towards better understanding and managing chronic pain.
